Fat-related Diet Habits Questionnaire
Abstract
The aim of this systematic review was to identify and describe brief dietary assessment tools suitable for use in clinical practice in the management of obesity, cardiovascular disease and type 2 diabetes. Papers describing development of brief (<35 items) dietary assessment questionnaires, that were accessible, simple to score and assessed aspects of the diet of relevance to the conditions of interest were identified from electronic databases. The development of 35 tools was described in 47 papers. Ten tools assessed healthy eating or healthy dietary patterns, 2 assessed adherence to the Mediterranean diet, 18 assessed dietary fat intake, and 5 assessed vegetable and/or fruit intake. Twenty tools were developed in North America. Test-retest reliability was conducted on 18 tools; correlation coefficients for total scores ranged from 0.59 to 0.95. Relative validation was conducted on 34 tools. The most common reference variable was percentage energy from fat (15 tools) and correlation coefficients ranged from 0.24, P<0.001 to 0.79, P<0.002. Tools that have been evaluated for reliability and/or relative validity are suitable for guiding clinicians when providing dietary advice. Variation in study design, settings and populations makes it difficult to recommend one tool over another, although future developers can enhance the understanding and use of tools by giving clear guidance as to the strengths and limitations of the study design. When selecting a tool, clinicians should consider whether their patient population is similar in characteristics to the evaluation sample.
Introduction
The World Health Organization estimates that in 2008, 18.3 million deaths worldwide were due to cardiovascular disease and type 2 diabetes.1 In 2010, unhealthy dietary habits, including low fruit and vegetable consumption, high salt intake and low whole-grain and fish consumption, combined with physical inactivity, are estimated to account for 10% of the global burden of disease. Assisting people with dietary modification is, therefore, a key challenge for health professionals.
In clinical care, dietary assessment is important for providing individualised dietary advice2 and is essential for evaluating the success of interventions aimed at improving dietary habits, such as cardiac rehabilitation programs.3 Dietitians typically use food diaries and take diet histories to obtain an overview of a patient's usual diet, with dietary advice then given based on this assessment. This process is time-consuming and interpretation requires specialist skills.2 However, a highly detailed assessment of nutrient intake is not always necessary in a clinical setting. It is often enough to review an individual's dietary habits to determine the potential benefit of changing specific dietary behaviours and foods/food groups.4
Brief dietary screening tools have been developed to assist with dietary assessment in clinical practice. These tools take the form of a brief questionnaire that can be self-completed prior to, or administered during, a consultation. The answers allow health professionals and patients to quickly identify whether a diet is appropriate or whether there are areas of concern. Dietary changes, based upon the patient's current dietary habits, can be discussed and food-based dietary goals set.5 For dietary tools to be useful in clinical practice, they need to be interpretable with minimal nutrition knowledge, quick to complete and easy to score. They must provide immediate guidance on healthy dietary changes or allow clinicians to quickly identify patients who may benefit from more intensive dietary counselling. Dietary screening tools have been designed to assess specific foods or nutrients,3, 6, 7 dietary behaviours associated with obesity8 or cardiovascular disease,9, 10, 11 adherence to specific diets12, 13 or as specific aids in dietary counselling with a prompt sheet provided to guide discussion.14, 15 They take the form of short food frequency questionnaires (FFQs), with16 or without17 portion estimates, behavioural questionnaires18 or a combination of FFQ and behavioural questions.7 They are unable to give estimates of absolute intake but can classify individuals as high, medium or low consumers of nutrients or foods of interest, allowing dietary advice to be targeted to an individual. Questionnaires have also been developed to rapidly evaluate the success of dietary interventions, for example, to measure the effect of advice to increase fruit and vegetable intake19 or follow a lipid-lowering diet.20 These are responsive to change and can provide outcome data to determine whether an intervention has succeeded in improving dietary habits. Brief questionnaires are of interest to dietary researchers,21 but the current review focuses on instruments that might be applicable in a clinical setting to obtain a picture of an individual's diet.
A review of brief dietary assessment tools for potential clinical use was published in 2000,22 but many additional tools have been developed since then and there is a need for an update. More recently, the US National Cancer Institute published an online registry of validated brief dietary assessment instruments.23 Although the registry provides an overview of the tools, it does not facilitate comparisons and provides no summarised information about applicability to clinical practice.
Our aims were to: (i) identify and describe available brief dietary screening tools that can be used in clinical practice for the prevention and management of obesity, cardiovascular disease and type 2 diabetes in adults; (ii) examine the acceptability, reliability and/or relative validity of the tools; and (iii) summarise the data so that clinicians can quickly assess which tool is most suitable for use with their patient group. Details are also provided about the availability of the tools and whether there are costs associated with their use.
Methods
Search strategy
Electronic databases MEDLINE, EMBASE, PsycINFO, AMED (Ovid versions) and CINAHL (EBSCOhost version) to June 2013 (week 26) were searched using MeSH terms and text words. Search terms were based around general terms for nutritional and dietary assessment, and were designed to identify brief questionnaires. Terms included nutrition assessment, diet screen, food questionnaire, nutrient questionnaire and short, brief, rapid and adult. The full list of search terms is included in the Supplementary Information (Appendix 1). One author (CE) screened all titles and abstracts. Full text articles were retrieved if abstracts appeared to meet the inclusion criteria. Additional studies were identified from reference lists and screened similarly. Studies were initially assessed for inclusion by one author (CE). Where it was unclear whether a study or questionnaire met the inclusion criteria a second author (JT) screened the reports.
Inclusion and exclusion criteria
Dietary habits or foods relevant to adults at risk for cardiovascular disease, overweight, obesity or type 2 diabetes were derived from national and international guidelines.24, 25, 26 Risk increases with high consumption of energy-dense foods, trans-fats, saturated fats, sodium and alcohol, and decreases with high consumption of high fibre foods, fruit and vegetables, fish and low glycaemic index foods. Dietary patterns emphasising high fibre foods, low fat dairy, poultry, fish, non-tropical vegetable oils and nuts, whereas limiting red and processed meats and high fat or sugar foods and drinks, are advised. Questionnaires assessing components of the diet that increase or decrease risk were identified.
Tools were included if they had been evaluated for reliability or relative validity against a biomarker or against another self-reported measure of dietary intake (dietary reference). In common with the previous review,22 sample size was not considered. On the basis of the clinical expertise of two authors (CE, RA), tools were deemed to be practical for clinical settings if they were brief, available in paper format or freely accessible on the Internet, could be scored at administration without specialist computer software and were capable of providing immediate feedback to patients and practitioners on an individual level. Questionnaires were defined as 'brief' if they were estimated to take no more than 15 min to complete. Mean allocated appointment times for new patients in primary care have been reported as being between 16 and 32 min and complete physicals as 12–36 min.27 Consequently, questionnaires taking more than 15 min to complete were judged as not feasible for use in clinical practice. However, most studies did not estimate completion time. Preliminary work, prior to conducting the full review, identified mean completion times of 15 min for a 25-item questionnaire,28 10 min for 31-item,29 20-item9 and 16-item10 questionnaires and 5–10 min for a 29-item questionnaire.5 Taking these measures into account, it was estimated that questionnaires of up to 35 items could feasibly be completed in 15 min. Tools designed to be administered by a practitioner or completed independently by the patient were both included.
Tools that assessed micronutrient intakes, protein intake, malnutrition screening tools or those aimed at identifying hazardous drinking were excluded. Questionnaires for single food groups, such as oily fish and pulses and fruit and vegetable questionnaires containing over 10 items, were considered to be of limited use in clinical practice and were excluded. Studies were excluded if they only reported the use of a questionnaire during an intervention or observational study, or described tools that were not tested for either reliability or relative validity. Owing to the limitations of time and cost, studies not published in English were excluded. It was not possible to obtain copies of two tools, despite contacting the institutions where they were developed, so these tools were excluded from the review.30, 31 A full list of inclusion and exclusion criteria is available in the Supplementary Information (Appendix 1).
Data extraction
The data extraction form was developed by all authors and piloted with four studies. One author (CE) extracted data from all studies. Data from 25% of studies were also extracted by an independent reviewer for cross-checking.
Study characteristics
The following data were extracted: study design, study setting, sample size, population and country. Age, gender, socio-economic status, education, disease state and ethnicity may all impact on the results of a relative validation study.32 As such, the sample profiles were categorised.
Questionnaire characteristics
Data were collected on the number of items, type of questions, scoring system and the language of the tool, the method of administration and whether the tool was designed for a specific population or for use in a particular setting.
Questionnaire items
Data were extracted on item generation as it is important to know whether a questionnaire has been tailored to the population of interest.4 Data were extracted on whether a questionnaire had been tested for acceptability (face validity, ease of use or an assessment of usefulness) and readability.
Reliability and relative validity
Results were extracted from test-retest reliability studies determining whether tools were consistent over two or more administrations,33 and from internal reliability studies determining whether items measuring the same dietary characteristic were consistent within a tool.34 Data from relative validity studies were extracted. In true validation studies, a new measure is compared with an accurate measurement of the truth, but this is very difficult for habitual diet.35 The gold standard for dietary intake is a recovery biomarker such as doubly labelled water, for energy intake, or urinary nitrogen for protein.36 These are expensive to administer, only available for a limited number of nutrients and inappropriate for brief questionnaires that do not measure the whole diet. Even direct observation is unsuitable as a true measure of habitual diet in free living individuals owing to the need for 24-h, possibly covert, surveillance. Consequently, short dietary assessment tools are evaluated against imperfect reference measures. These include self-reported dietary measures, for example, food diaries, a longer FFQ or 24-h recalls; a concentration biomarker such as plasma vitamin levels,37 or biomarkers of pre-clinical disease38 such as blood lipids or anthropometric measures. None of these are true measures of habitual intake. Dietary measures are subject to measurement error, which vary depending upon the method. For example, those reliant on memory, such as FFQs, are subject to recall bias, whereas food records can change dietary behaviour.4 The use of food tables for nutrient analysis further introduces error in both self-report and direct observation of diet.35 Furthermore, if errors in the reference measure correlate with errors in the new measure, for example, if both methods are subject to recall bias, relative validity of the new measure could be overestimated.35 Concentration biomarkers and biomarkers of pre-clinical disease are affected by metabolic and lifestyle factors. For example, levels of plasma β-carotene are not only determined by dietary intake but also by fat intake, body mass index (BMI), low-density lipoprotein levels and smoking.37 However, these biomarkers can provide additional evidence of accuracy of a questionnaire when used in conjunction with other reference measures.
Internal reliability is typically tested using Cronbach's α, which assesses how closely items correlate with each other.34 Values of >0.70 indicate high internal reliability, although strong correlation between items in a dietary questionnaire may not be required if each item is designed to assess different aspects of the diet.39 Test-retest reliability and relative validity are commonly tested at the individual level using correlation statistics.35 The use of mean values alone can only assess these at the group level.40 Correlation coefficients of ⩾0.4 for the nutrient of interest are considered to be adequate for FFQs when compared with another dietary reference measure.4 Correlations of ⩽0.4 are more usual when FFQs are compared with a biomarker.37 Studies calibrating long FFQs against other dietary assessment methods, such as food diaries, have reported coefficients between −0.16 and 0.86 for total fat in grams (mean 0.51), −0.01 and 0.71 for fruit and 0.16 and 0.72 for vegetables.41 Test-retest reliability studies for long FFQs quote coefficients of 0.50–0.70 for energy, fat and selected micronutrients.41
The practice of only examining the correlations between scores to determine test-retest reliability or validity has been criticised, and it has been recommended that the Bland Altman method be used in conjunction.33 Details of the statistical tests used were summarised.
Results
A total of 1802 separate records were identified, 1795 via the electronic databases and a further 7 from hand searching references. One hundred and twenty-two full text papers were screened and 47 met the inclusion criteria (Figure 1). The development and testing of 35 tools were described in these papers, although 2, the Block Fat, Fruit and Vegetable Screeners (B-F&FV)6 and the Hispanic Fat, Fruit and Vegetable Screeners (H-F&FV),42 can be split into two distinct sets of questions that provide scores for different aspects of the diet. In addition, two different versions of two tools, the Rapid Eating Assessment for Patients (REAP29 and REAP-S14) and the Food Behaviour Checklist (FBC-T10 and FBC-V43), are currently available, and the FBC-V has been translated into Spanish (FBC-SV) and evaluated32, 44 One, the Fat Related Diet Habits Questionnaire (FRDHQ), appears to have been used in several different versions. Papers describing the relative validity testing of the 20-item and 24-item questionnaires are detailed here21, 45, 46, 47 although 21-48 and 23-item49 versions have been used in interventions. The current version, available online, contains 25 distinct items (http://sharedresources.fhcrc.org/documents/fat-related-questionnaire). For the purposes of this review, B-F&FV and H-F&FV were regarded as single tools, REAP and REAP-S and FBC-T and FBC-V were regarded as distinct tools, with FBC-SV as a subsidiary to FBC-V. All the versions of FRDHQ were regarded as one tool.
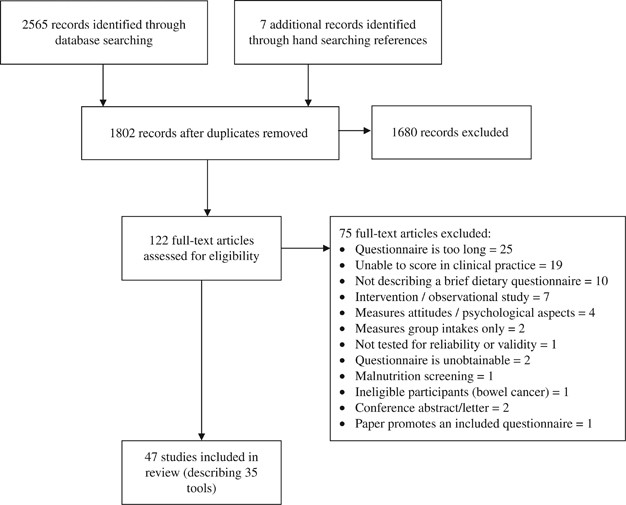
Prisma diagram. Brief dietary questionnaires.
Full size image
Table 1 summarises the study and tool characteristics. Over half (n=20) were developed and tested in the USA or Canada with the remainder in European countries (n=10) and Australia or New Zealand (n=5).
Full size table
Dietary assessment
Fifteen papers described 10 tools assessing healthy eating or healthy dietary patterns8, 10, 13, 14, 28, 29, 32, 43, 44, 50, 51, 52, 53, 54, 55 and 2 assessing adherence to the Mediterranean diet.13, 56 Twenty-four papers described 18 tools providing information on the intake of dietary fats or dietary behaviours associated with fat intake. Of these, 11 were specific for dietary fats alone,3, 12, 15, 20, 21, 39, 45, 46, 47, 57, 58, 59, 60, 61, 62, 63, 64 1 assessed dietary fat and free sugars,65 4 assessed dietary fat and fibre intakes5, 7, 9, 18 and 2 assessed dietary fat and fruit and vegetable intake (although these can be used separately as one screener for fat and one for fruit and vegetables).6, 42 Four tools assessed fruit and vegetable intake16, 17, 19, 66, 67 and one assessed fruit intake alone.68 With the exception of questionnaires specific for fruit and vegetable intake, no tool was designed to characterise diets by food groups, although three broader tools also provided a fruit and vegetable sub-score.10, 43, 50
Fifteen tools were short FFQs and asked questions on the frequency of consumption of specific foods.3, 5, 6, 12, 13, 42, 58, 60, 69 All of the fruit and vegetable questionnaires were in this form.16, 17, 19, 66, 68 Four exclusively asked about food behaviours, for example, 'In the past month how often did you eat fish or chicken instead of red meat?' or, 'In an average week, how often do you skip breakfast?'14, 18, 29, 45 The remaining 16 contained a mixture of FFQ and behavioural questions.7, 8, 9, 10, 15, 20, 28, 39, 44, 50, 54, 55, 56, 57, 59, 61
All except six8, 10, 14, 29, 44, 52, 55 were scored numerically, with a total score or subscales for separate nutrients or fruit and vegetable intakes. The six that were not scored in this manner give individual guidance for each item, and two14, 29 also provide a prompt sheet to aid advice.
Item generation
Item generation was described for 27 tools, with 8 employing more than one method. Fourteen were adapted from longer FFQs and other questionnaires,3, 7, 12, 14, 15, 18, 20, 39, 43, 50, 54, 56, 59, 69 of which six were initially based upon other tools included in this review.14, 15, 18, 20, 43, 54 Six used national databases to identify foods most commonly consumed from a particular category, or foods that contributed most to the nutrient of interest in the population of interest.5, 42, 54, 57, 68, 69 Seven used recommendations or clinical guidelines5, 10, 29, 53, 55, 56, 58 and four were developed using an expert panel.9, 10, 45, 53 Five were developed from data collected from participants, either quantitative in the form of dietary patterns51 or through qualitative work.10, 18, 42, 54
Fourteen reported being evaluated in some way for acceptability to check that wording was clear, questions were relevant and the general layout of the tool was appropriate. Four employed cognitive interviewing,29, 32, 43, 51, 68 three used survey methods,7, 50, 55 five used unspecified qualitative interviews10, 18, 42, 53, 58 and two used unspecified pilot testing.20, 59 Only the FBC-T and the visual versions derived from it were evaluated for reading comprehension.32, 43, 52 The FBC-T and FBC-SV were of low reading difficulty and the colour version of the FBC-SV was 'very easy'.
Reliability and relative validity
Table 2 summarises the results of reliability and relative validity studies. Just over half the tools (n=18) were tested for test-retest reliability,7, 9, 18, 19, 20, 29, 39, 42, 44, 52, 55, 57, 58, 59, 60, 61, 69 with one being tested in three different samples.21, 45, 47 Test-retest time varied from several hours7 to 1 year18, 19, 57 and different studies employed different statistical tests, although correlations were most often used (14 tools).7, 9, 18, 19, 20, 29, 39, 42, 44, 45, 52, 55, 57, 59 Test-retest correlation coefficients for total scores ranged from 0.5921 to 0.95.7 Four studies did not calculate a total score but used individual items, group classifications or derived nutrient intakes from the screener as test-retest variables.52, 55, 58, 60 One study61 was evaluated exclusively at the group level. Internal reliability was tested in nine tools3, 8, 39, 44, 54, 58, 69 with two employing more than one sample.10, 45, 46, 47, 52 Values for Cronbach's α were reported from 0.47 54 to 0.83.47All tools were examined for relative validity at the individual level against a reference measure except one.42 A number of different reference measures, with a range of different times between tests, different test variables and different statistical tests were used to determine relative validity. No study employed a recovery biomarker. Nine tools were compared with an FFQ that had previously reported relative validity against food diaries or dietary recalls6, 9, 14, 15, 18, 55, 59, 60, 66 and 13 were compared with food diaries,5, 16, 50, 57, 61 recalls13, 17, 44, 54, 67 or a diet history.58, 68 One was compared with a different brief questionnaire that had been previously tested for relative validity against 24 h recalls.39 Nine tools were compared with more than one reference measure;8, 10, 12, 20, 21, 28, 29, 45, 46, 47, 52, 53, 56, 62, 63, 64, 69 and three were compared with more than one dietary reference.12, 21, 29, 45, 46, 47, 62, 63, 64 Alongside a dietary reference, four10, 28, 56, 58 were compared with biomarkers of preclinical disease, four28, 53, 56, 69 with anthropometric measures, and two10, 28 with concentration biomarkers. Two did not use a dietary reference measure but compared change in total score with change in BMI3 and change in total score with change in plasma carotenoids and plasma vitamin C.19 The variation in study designs makes direct comparisons between tools problematic, but total score (or fat score) from 11 tools5, 9, 12, 15, 18, 20, 21, 29, 45, 46, 47, 54, 59, 62, 63, 64, 65 were reported to have been compared with % energy from total fat from food diaries or FFQs. Correlation coefficients ranged from 0.2446 to 0.79.12 Total scores from two of these tools were compared with % energy from total fat from a dietary reference in more than one population: the FRDHQ reported correlation coefficients ranging from 0.2446 to 0.6045 and MEDFICTS from 0.3063 to 0.79.12
Full size table
Table 3 gives an 'at a glance' summary of the characteristics of each tool, the evaluation studies and provides information on access.
Full size table
Discussion
Main findings
This systematic review identified 35 tools with potential application to dietary assessment in clinical settings. Around half assess dietary fat intake, with or without other nutrients, a third assess the overall diet for healthy eating or adherence to the Mediterranean diet, and the remainder assess fruit and vegetable intake. More tools have been developed and evaluated in the USA than in any other country.
Fewer than half the tools reported evaluations for clarity of language and acceptability with users. Owing to the variation in methodology, it is not possible to determine whether the tools that were evaluated for acceptability show greater reliability or relative validity than those that were not. However, best practice in FFQ design involves pre-testing.41
All tools, except one, were tested for relative validity against one or more reference measures, although there was a wide variation in the design of studies, the variables used and the statistical tests employed. Three quarters were tested against a different dietary reference measure, with over a quarter using a FFQ or a different brief questionnaire. As the majority of brief questionnaires were themselves FFQs, or included many food frequency questions, errors between the tools and the FFQs may have been correlated and the relative validity of these questionnaires overestimated. Around half were evaluated for test-retest reliability with similar variation in study design. This variation makes direct comparison between tools difficult, and as a consequence, it is not possible to state that one tool is superior for a particular nutrient or population. However, correlation coefficients for relative validity against food diaries and biomarkers and those for reliability studies are similar to those obtained in studies that evaluate longer FFQs against food diaries. This indicates that these brief dietary screening tools can be expected to produce a fair approximation of dietary habits and consequently could be of use in clinical practice for the dietary management of cardiovascular disease, obesity and type 2 diabetes. It is worth noting, however, that few tools reported sensitivity, specificity or predictive values28 55, 62, 63, 64, 66, 68 and only six (17%) have assessed sensitivity to change over time;3, 18, 19, 20, 39, 54 therefore, their utility in an intervention setting is unclear.
Strengths and limitations of the review
The strengths of this review are the application of a systematic search strategy and systematic data extraction techniques. Dietary assessment tools developed since the review by Calfas et al. 22 in 2000 and validated tools that are not listed in the NIC registry have been identified and described. Tools that were not included in study reports were obtained online or from the original authors to ensure they met the inclusion criteria. The results are presented so that clinicians and researchers can select available tools that are most suitable for their purposes.
The review has some important limitations. The piloting and use of dietary screening tools in practice has not been examined, which means it is not possible to determine whether use of a tool has a positive effect on patient behaviour. The inclusion and exclusion criteria were developed for this review and assessment of whether a tool would be useful in clinical practice was derived from the expert opinion of only two clinicians. Other reviewers or clinicians may disagree with the criteria and may have included or excluded different brief tools. Calfas et al. 22 judged that tools suitable for use in primary care would take 15 min to complete or be around 50-items long but provided no justification for this. The current review based an estimate of completion time on preliminary data obtained from brief dietary questionnaires. We excluded tools assessing single food groups because there is limited clinical benefit in a detailed assessment of one food group, with the exception of fruit and vegetable intake. However, fruit and vegetable questionnaires of greater than 10 items were excluded because increased patient burden reduces feasibility in clinical practice. Only peer-reviewed studies published in English were included. There may be evaluated tools that are used in clinical practice in other countries, or that have not been peer-reviewed that have not been identified here. However, owing to the heterogeneity of studies, this would be unlikely to change the broader conclusions of this review.
Comparison with other studies
The review by Calfas et al. 22 used wider inclusion criteria than this current review and did not consider whether a tool could be easily scored in practice. They identified 14 dietary assessment tools, of which 7 are included in the present review.5, 6, 11, 12, 15, 20, 55 All measured dietary fat, making comparisons between tools more straightforward. Four were evaluated for test-retest reliability, with correlation coefficients ranging from 0.67 to 0.91. The 11 validated tools were either validated against a food diary or a longer FFQ, and correlation coefficients for % energy from fat ranged from 0.30 to 0.80. These ranges are similar to coefficients reported in the current review.
In 2003, Kim et al. 70 reviewed tools reported as validated, containing up to 16 items, and designed to assess fruit and vegetable intake. They identified 10 instruments, of which 1 is included in the current review.17 The remainder were excluded in the current review for reasons of length or because the scoring algorithms were complex and unlikely to be used in clinical practice. Tools were reported as validated against longer FFQs, food diaries or 24-h recalls. Correlation coefficients for total fruit and vegetable intakes ranged from 0.29 to 0.80. As the tools measured the same aspect of the diet, comparisons were possible and this review concluded that more detailed tools that asked about portion sizes and the consumption of mixed vegetable dishes showed greater relative validity. Cade et al. 41 also comment that FFQs asking people to estimate their own portion sizes are more reliable. Only one tool included in the current review asks people to estimate their portion sizes by providing a multiple choice list of three different sizes.12
All the studies previously reviewed used correlations alone to assess reliability and relative validity. This remains the most common method, and only five studies in the present review made use of the Bland–Altman method. Correlation coefficients are not measures of absolute agreement but are instead measures of relative agreement, assessing whether an individual has maintained their ranking relative to other participants. The intra-class correlation coefficient was used to evaluate four tools, but this measure has also been criticised and data simulations have shown that high correlations can be achieved with low absolute agreement.71 The Bland–Altman method assesses limits of agreement that define the range that 95% of the differences between the measures lie within, and may include graphical presentation of the data. Clinical knowledge must be used to decide if the limits of agreement are acceptable.72 Of the studies that used the Bland–Altman method, one was published in 20027 and the remainder after 2010, with three studies conducted by the same team.13, 56, 68
Clinical implications
It is important that clinicians are clear about their purpose when selecting a tool for use. In clinical practice, dietary assessment is required to assist in the provision of dietary advice or to measure the impact of dietary intervention.4 Brief dietary questionnaires used for the former purpose are those that give clear guidance on moving to healthier dietary habits rather than obtaining a detailed, quantitative assessment of an individual's diet. Assessment may be focussed on certain nutrients to be disease-specific or may be concerned with overall diet quality. Typical questions from tools included in the current review include asking about the frequency of consumption of sweet foods or savoury snacks, with responses ranging from less than once a week to more than three times a day. The answers can be used to target dietary advice to the individual. Tools suitable for measuring the impact of a dietary intervention must also be able to measure change.
This review provides evidence that tools developed and tested in one population may not have the same relative validity in a different population. Equally, tools developed in different countries will include different food items, also affecting relative validity. It should be noted that English translations of tools developed in Spanish, French, Norwegian or Dutch have not been validated and that older tools may no longer be appropriate because of shifts in food habits and processing.73 In common with previous reviews,22, 70 studies with small sample sizes were not excluded. Cade et al. 41 report a wide range of sample sizes for relative validation studies of long FFQs and found no difference in reported correlation coefficients between studies with large sample sizes compared with small sample sizes. However, with small sample sizes, confidence intervals are likely to be wide and consequently sample sizes of around 100–200 are advised.40 Clinicians should consider the sample sizes of test-retest and relative validation studies if tools are to be used 'off the shelf'.
Developers of future tools can enhance understanding of the development, relative validity and reliability of tools by clearly describing: (i) how items were derived; (ii) the population of interest; (iii) the characteristics of the sample for reliability and relative validation studies; (iv) the results of these studies; and (v) whether stratification by age, gender, ethnicity and socioeconomic status affected results. Tools that are most helpful for clinical use need to have a clearly described and simple scoring system, and ideally a copy presented in the paper or in an online appendix for evaluation with clear information about copyright. Table 4 provides a checklist to assist practitioners when choosing a brief dietary questionnaire for clinical use.
Full size table
Conclusion
This review identified and summarised 35 short dietary assessment tools of potential use in clinical practice for the dietary management of cardiovascular disease, obesity and type 2 diabetes. In general, tools demonstrated adequate reliability and/or relative validity, although around half have been developed and evaluated exclusively in US populations. It is not possible to determine whether any one tool is clearly better than another for a given population or purpose owing to differences in the design of reliability and relative validity studies. If tools are to be used in different countries or populations, they need to be adapted and evaluated locally to ensure they are reliable and have acceptable levels of relative validity.
References
- 1
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380: 2224–2260.
Article Google Scholar
- 2
Thomas B, Bishop J . Manual of Dietitic Practice4th EditionJohn Wiley and Sons Ltd: Chicester, 2007.
Google Scholar
- 3
Anderson CAM, Kumanyika SK, Shults J, Kallan MJ, Gans KM, Risica PM . Assessing change in dietary-fat behaviors in a weight-loss program for African Americans: a potential short method. J Am Diet Assoc 2007; 107: 838–842.
Article Google Scholar
- 4
Thompson FE, Byers T . Dietary Assessment Resource Manual. J Nutr 1994; 124 (11 Suppl), 2245s–2317s.
CAS PubMed Google Scholar
- 5
Roe L, Strong C, Whiteside C, Neil A, Mant D . Dietary intervention in primary care: Validity of the DINE method for diet assessment. Fam Pract 1994; 11: 375–381.
CAS Article Google Scholar
- 6
Block G, Gillespie C, Rosenbaum EH, Jenson C . A rapid food screener to assess fat and fruit and vegetable intake. Am J Prev Med 2000; 18: 284–288.
CAS Article Google Scholar
- 7
Svilaas A, Strom EC, Svilaas T, Borgejordet A, Thoresen M, Ose L . Reproducibility and validity of a short food questionnaire for the assessment of dietary habits. Nutr Metab Cardiovasc Dis 2002; 12: 60–70.
CAS PubMed Google Scholar
- 8
Greenwood JLJ, Lin J, Arguello D, Ball T, Shaw JM . Healthy eating vital sign: a new assessment tool for eating behaviors. ISRN Obes 2012; 2012: 7.
Google Scholar
- 9
Wright JL, Scott JA . The Fat and Fibre Barometer, a short food behaviour questionnaire: reliability, relative validity and utility. Australian Journal of Nutrition & Dietetics 2000; 57: 33–39.
Google Scholar
- 10
Murphy SP, Kaiser LL, Townsend MS, Allen LH . Evaluation of validity of items for a food behavior checklist. J Am Diet Assoc 2001; 101: 751–761.
CAS Article Google Scholar
- 11
Kristal AR, Shattuck AL, Henry HJ . Patterns of dietary behavior associated with selecting diets low in fat: reliability and validity of a behavioral approach to dietary assessment. J Am Diet Assoc 1990; 90: 214–220.
CAS PubMed Google Scholar
- 12
Kris-Etherton P, Eissenstat B, Jaax S, Srinath UMA, Scott L, Rader J et al. Validation for MEDFICTS, a Dietary Assessment Instrument for Evaluating Adherence to Total and Saturated Fat Recommendations of the National Cholesterol Education Program Step 1 and Step 2 Diets. J Am Diet Assoc 2001; 101: 81–86.
CAS Article Google Scholar
- 13
Schroder H, Benitez Arciniega A, Soler C, Covas M-I, Baena-Diez JM, Marrugat J . Validity of two short screeners for diet quality in time-limited settings. Public Health Nutr 2012; 15: 618–626.
Article Google Scholar
- 14
Segal-Isaacson CJ, Wylie-Rosett J, Gans KM . Nutrition update. Validation of a short dietary assessment questionnaire: the Rapid Eating and Activity Assessment for Participants Short Version (REAP-S). Diabetes Educ 2004; 30: 774.
CAS Article Google Scholar
- 15
Gans KM, Sundaram SG, McPhillips JB, Hixson ML, Linnan L, Carleton RA . Rate your plate: An eating pattern assessment and educational tool used at cholesterol screening and education programs. J Nutr Educ 1993; 25: 29–36.
Article Google Scholar
- 16
Van Assema P, Brug J, Ronda G, Steenhuis I, Oenema A . A short dutch questionnaire to measure fruit and vegetable intake: relative validity among adults and adolescents. Nutr Health 2002; 16: 85–106.
Article Google Scholar
- 17
Thompson FE, Kipnis V, Subar AF, Krebs-Smith SM, Kahle LL, Midthune D et al. Evaluation of 2 brief instruments and a food-frequency questionnaire to estimate daily number of servings of fruit and vegetables. Am J Clin Nutr 2000; 71: 1503–1510.
CAS Article Google Scholar
- 18
Shannon J, Kristal AR, Curry SJ, Beresford SA . Application of a behavioral approach to measuring dietary change: the fat- and fiber-related diet behavior questionnaire. Cancer Epidemiol Biomarkers Prev 1997; 6: 355–361.
CAS PubMed Google Scholar
- 19
Bogers RP, Van Assema P, Kester ADM, Westerterp KR, Dagnelie PC . Reproducibility, validity, and responsiveness to change of a short questionnaire for measuring fruit and vegetable intake. Am J Epidemiol 2004; 159: 900–909.
Article Google Scholar
- 20
Retzlaff BM, Dowdy AA, Walden CE, Bovbjerg VE, Knopp RH . The Northwest Lipid Research Clinic Fat Intake Scale: validation and utility. Am J Public Health 1997; 87: 181–185.
CAS Article Google Scholar
- 21
Glasgow RE, Perry JD, Toobert DJ, Hollis JF . Brief assessments of dietary behavior in field settings. Addict Behav 1996; 21: 239–247.
CAS Article Google Scholar
- 22
Calfas KJ, Zabinski MF, Rupp J . Practical nutrition assessment in primary care settings: a review. Am J Prev Med 2000; 18: 289–299.
CAS Article Google Scholar
- 23
National Cancer Institute Register of Validated Short Dietary Assessment Instruments. National Institutes of Health, 2013, Available from http://appliedresearch.cancer.gov/diet/shortreg/ (Accessed 11 February 2015).
- 24
Eckel RH, Jakicic JM, Ard JD, Miller NH, Hubbard VS, Nonas CA et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; 63 (25 Pt B), 2960–2984.
PubMed Google Scholar
- 25
Dyson PA, Kelly T, Deakin T, Duncan A, Frost G, Harrison Z et alDiabetes UK Nutrition Working Group. Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes. Diabet Med 2011; 28: 1282–1288.
CAS Article Google Scholar
- 26
WHO/FAO Diet, nutrition and the prevention of chronic diseases 2002: World Health Organisation: Geneva.
- 27
Konrad TR, Link CL, Shackelton RJ, Marceau LD, von dem Knesebeck O, Siegrist J et al. It's about time: physicians' perceptions of time constraints in primary care medical practice in three national healthcare systems. Med Care 2010; 48: 95–100.
Article Google Scholar
- 28
Bailey RL, Miller PE, Mitchell DC, Hartman TJ, Lawrence FR, Sempos CT et al. Dietary screening tool identifies nutritional risk in older adults. Am J Clin Nutr 2009; 90: 177–183.
CAS Article Google Scholar
- 29
Gans KM, Risica PM, Wylie-Rosett J, Ross EM, Strolla LO, McMurray J et al. Development and evaluation of the nutrition component of the Rapid Eating and Activity Assessment for Patients (REAP): a new tool for primary care providers. J Nutr Educ Behav 2006; 38: 286–292.
Article Google Scholar
- 30
Ling AM, Horwath C, Parnell W . Validation of a short food frequency questionnaire to assess consumption of cereal foods, fruit and vegetables in Chinese Singaporeans. Eur J Clin Nutr 1998; 52: 557–564.
CAS Article Google Scholar
- 31
Peters JR, Quiter ES, Brekke ML, Admire J, Brekke MJ, Mullis RM et al. The eating pattern assessment tool: A simple instrument for assessing dietary fat and cholesterol intake. J Am Diet Assoc 1994; 94: 1008–1013.
CAS Article Google Scholar
- 32
Banna JC, Vera Becerra LE, Kaiser LL, Townsend MS . Using qualitative methods to improve questionnaires for Spanish speakers: assessing face validity of a food behavior checklist. J Am Diet Assoc 2010; 110: 80–90.
Article Google Scholar
- 33
Cade J, Thompson R, Burley V, Warm D . Development, validation and utilisation of food-frequency questionnaires – a review. Public Health Nutr 2002; 5: 567–587.
Article Google Scholar
- 34
Gleason PM, Harris J, Sheean PM, Boushey CJ, Bruemmer B . Publishing nutrition research: validity, reliability, and diagnostic test assessment in nutrition-related research. J Am Diet Assoc 2010; 110: 409–419.
Article Google Scholar
- 35
Block G, Hartman AM . Issues in reproducibility and validity of dietary studies. Am J Clin Nutr 1989; 50: 1133–1138.
CAS Article Google Scholar
- 36
Freedman LS, Commins JM, Moler JE, Arab L, Baer DJ, Kipnis V et al. Pooled results from 5 validation studies of dietary self-report instruments using recovery biomarkers for energy and protein intake. Am J Epidemiol 2014; 180: 172–188.
Article Google Scholar
- 37
Kaaks RJ . Biochemical markers as additional measurements in studies of the accuracy of dietary questionnaire measurements: conceptual issues. Am J Clin Nutr 1997; 65: 1232S–1239S.
CAS Article Google Scholar
- 38
Arab L, Akbar J . Biomarkers and the measurement of fatty acids. Public Health Nutr 2002; 5: 865–871.
Article Google Scholar
- 39
Paxton AE, Strycker LA, Toobert DJ, Ammerman AS, Glasgow RE . Starting the conversation: performance of a brief dietary assessment and intervention tool for health professionals. Am J Prev Med 2011; 40: 67–71.
Article Google Scholar
- 40
Willett WC (ed). Nutritional Epidemiology 2nd edition. Oxford University Press Inc.: New York, 1998.
- 41
Cade JE, Burley VJ, Warm DL, Thompson RL, Margetts BM . Food-frequency questionnaires: a review of their design, validation and utilisation. Nutr Res Rev 2004; 17: 5–22.
CAS Article Google Scholar
- 42
Wakimoto P, Block G, Mandel S, Medina N . Development and reliability of brief dietary assessment tools for Hispanics. Prev Chronic Dis 2006; 3: A95.
PubMed PubMed Central Google Scholar
- 43
Townsend MS, Sylva K, Martin A, Metz D, Wooten-Swanson P . Improving readability of an evaluation tool for low-income clients using visual information processing theories. J Nutr Educ Behav 2008; 40: 181–186.
Article Google Scholar
- 44
Banna JC, Townsend MS . Assessing factorial and convergent validity and reliability of a food behaviour checklist for Spanish-speaking participants in US Department of Agriculture nutrition education programmes. Public Health Nutr 2011; 14: 1165–1176.
Article Google Scholar
- 45
Kristal AR, Abrams BF, Thornquist MD, Disogra L, Croyle RT, Shattuck AL et al. Development and validation of a food use checklist for evaluation of community nutrition interventions. Am J Public Health 1990; 80: 1318–1322.
CAS Article Google Scholar
- 46
Birkett NJ, Boulet J . Validation of a food habits questionnaire: poor performance in male manual laborers. J Am Diet Assoc 1995; 95: 558–563.
CAS Article Google Scholar
- 47
Spoon MP, Devereux PG, Benedict JA, Leontos C, Constantino N, Christy D et al. Usefulness of the food habits questionnaire in a worksite setting. J Nutr Educ Behav 2002; 34: 268–272.
Article Google Scholar
- 48
Kristal AR, Curry SJ, Shattuck AL, Feng Z, Li S . A randomized trial of a tailored, self-help dietary intervention: The Puget Sound Eating Patterns Study. Prev Med 2000; 31: 380–389.
CAS Article Google Scholar
- 49
Kristal AR, Shattuck AL, Patterson RE . Differences in fat-related dietary patterns between black, Hispanic and white women: results from the Women's Health Trial Feasibility Study in Minority Populations. Public Health Nutr 1999; 2: 253–262.
CAS Article Google Scholar
- 50
O'Reilly SL, McCann LR . Development and validation of the Diet Quality Tool for use in cardiovascular disease prevention settings. Aust J Prim Health 2012; 18: 138–147.
CAS Article Google Scholar
- 51
Bailey RL, Mitchell DC, Miller CK, Still CD, Jensen GL, Tucker KL et al. A dietary screening questionnaire identifies dietary patterns in older adults. J Nutr 2007; 137: 421–426.
CAS Article Google Scholar
- 52
Townsend MS, Kaiser LL, Allen LH, Joy AB, Murphy SP . Selecting items for a food behavior checklist for a limited-resource audience. J Nutr Educ Behav 2003; 35: 69–77.
Article Google Scholar
- 53
Greenwood JLJ, Murtaugh MA, Omura EM, Alder SC, Stanford JB . Creating a clinical screening questionnaire for eating behaviors associated with overweight and obesity. J Am Board Fam Med 2008; 21: 539–548.
Article Google Scholar
- 54
Fernandez S, Olendzki B, Rosal MC . A dietary behaviors measure for use with low-income, Spanish-speaking Caribbean Latinos with type 2 diabetes: The Latino Dietary Behaviors Questionnaire. J Am Diet Assoc 2011; 111: 589–599.
Article Google Scholar
- 55
Rifas-Shiman SL, Willett WC, Lobb R, Kotch J, Dart C, Gillman MW . PrimeScreen, a brief dietary screening tool: reproducibility and comparability with both a longer food frequency questionnaire and biomarkers. Public Health Nutr 2001; 4: 249–254.
CAS Article Google Scholar
- 56
Schroder H, Fito M, Estruch R, Martinez-Gonzalez MA, Corella D, Salas-Salvado J et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J Nutr 2011; 141: 1140–1145.
CAS Article Google Scholar
- 57
Van Assema P, Brug J, Kok G, Brants H . The reliability and validity of a Dutch questionnaire on fat consumption as a means to rank subjects according to individual fat intake. Eur J Cancer Prev 1992; 1: 375–380.
CAS Article Google Scholar
- 58
Beliard S, Coudert M, Valero R, Charbonnier L, Duchene E, Allaert FA et al. Validation of a short food frequency questionnaire to evaluate nutritional lifestyles in hypercholesterolemic patients. Ann Endocrinol (Paris) 2012; 73: 523–529.
Article Google Scholar
- 59
Dobson AJ, Blijlevens R, Alexander HM, Croce N, Heller RF, Higginbotham N et al. Short fat questionnaire: a self-administered measure of fat-intake behaviour. Aust J Public Health 1993; 17: 144–149.
CAS Article Google Scholar
- 60
Kraschnewski JL, Gold AD, Gizlice Z, Johnston LF, Garcia BA, Samuel-Hodge CD et al. Development and evaluation of a brief questionnaire to assess dietary fat quality in low-income overweight women in the Southern United States. J Nutr Educ Behav 2013; 45: 355–361.
Article Google Scholar
- 61
Heller RF, Tunstall Pedoe HD, Rose G . A simple method of assessing the effect of dietary advice to reduce plasma cholesterol. Prev Med 1981; 10: 364–370.
CAS Article Google Scholar
- 62
Taylor A, Wong H, Wish K, Carrow J, Bell D, Bindeman J et al. Validation of the MEDFICTS dietary questionnaire: A clinical tool to assess adherence to American Heart Association dietary fat intake guidelines. Nutr J 2003; 2: 4.
Article Google Scholar
- 63
Teal CR, Baham DL, Gor BJ, Jones LA . Is the MEDFICTS rapid dietary fat screener valid for premenopausal African-American women? J Am Diet Assoc 2007; 107: 773–781.
Article Google Scholar
- 64
Mochari H, Gao Q, Mosca L . Validation of the MEDFICTS dietary assessment questionnaire in a diverse population. J Am Diet Assoc 2008; 108: 817–822.
Article Google Scholar
- 65
Francis H, Stevenson R . Validity and test–retest reliability of a short dietary questionnaire to assess intake of saturated fat and free sugars: a preliminary study. J Hum Nutr Diet 2013; 26: 234–242.
CAS Article Google Scholar
- 66
Godin G, Belanger-Gravel A, Paradis A-m, Vohl M-C, Perusse L . A simple method to assess fruit and vegetable intake among obese and non-obese individuals. Can J Public Health 2008; 99: 494–498.
PubMed Google Scholar
- 67
Kristal AR, Vizenor NC, Patterson RE, Neuhouser ML, Shattuck AL, McLerran D . Precision and Bias of Food Frequency-based Measures of Fruit and Vegetable Intakes. Cancer Epidemiol Biomarkers Prev 2000; 9: 939–944.
CAS PubMed Google Scholar
- 68
Mainvil LA, Horwath CC, McKenzie JE, Lawson R . Validation of brief instruments to measure adult fruit and vegetable consumption. Appetite 2011; 56: 111–117.
Article Google Scholar
- 69
Francis H, Stevenson R . Validity and test–retest reliability of a short dietary questionnaire to assess intake of saturated fat and free sugars: a preliminary study. J Hum Nutr Diet 2012; 26: 234–242.
Article Google Scholar
- 70
Kim DJ, Holowaty EJ . Brief, validated survey instruments for the measurement of fruit and vegetable intakes in adults: a review. Prev Med 2003; 36: 440–447.
Article Google Scholar
- 71
Atkinson G, Nevill A . Statistical methods for assessing measurement error (reliability) in variables relevant to sports medicine. Sports Med 1998; 26: 217–238.
CAS Article Google Scholar
- 72
Bland JM, Altman DG . Measuring agreement in method comparison studies. Stat Methods Med Res 1999; 8: 135–160.
CAS Article Google Scholar
- 73
Whitton C, Nicholson SK, Roberts C, Prynne CJ, Pot GK, Olson A et al. National Diet and Nutrition Survey: UK food consumption and nutrient intakes from the first year of the rolling programme and comparisons with previous surveys. Br J Nutr 2011; 106: 1899–1914.
CAS Article Google Scholar
Download references
Acknowledgements
We thank the developers of brief questionnaires who provided access to their questionnaires for evaluation, their scoring algorithms and supplementary information on usage and copyright. We thank Amir Emadian for independent data extraction on 25% of the included papers. Clare England is supported by NIHR Clinical Doctoral Research Fellowship 10-017. The study was carried out at The University of Bristol, Senate House, Tyndall Avenue, Bristol BS8 1TH.
Author Contributions
The work contained in this article is part of the PhD of Clare England which is supervised by Drs' Andrews, Jago and Thompson. All authors assisted in the design of the data extraction form and development of the search strategy. Ms England screened all titles and abstracts and extracted the data with advice on clinical application from Dr Andrews and final inclusion from Professor Thompson. Professor Jago provided analytical guidance. The first draft of the manuscript was prepared by Ms England with critical input and revisions by all other authors. All authors approved the final manuscript.
Declaration
This submission represents original work that has not been published previously and it is not being considered for publication elsewhere.
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on European Journal of Clinical Nutrition website
Supplementary information
Rights and permissions
About this article
Cite this article
England, C., Andrews, R., Jago, R. et al. A systematic review of brief dietary questionnaires suitable for clinical use in the prevention and management of obesity, cardiovascular disease and type 2 diabetes. Eur J Clin Nutr 69, 977–1003 (2015). https://doi.org/10.1038/ejcn.2015.6
Download citation
-
Received:
-
Revised:
-
Accepted:
-
Published:
-
Issue Date:
-
DOI : https://doi.org/10.1038/ejcn.2015.6
Further reading
Fat-related Diet Habits Questionnaire
Source: https://www.nature.com/articles/ejcn20156
0 Response to "Fat-related Diet Habits Questionnaire"
Post a Comment